With rapid advancements in medical technology reshaping healthcare, new devices and innovations are emerging faster than ever before. From innovative diagnostic tools to cutting-edge implants and wearable devices, these advancements hold immense potential. But with great innovation comes the need for heightened vigilance.How do we ensure that these devices, designed to save and improve lives, do not inadvertently introduce new risks? This is where technovigilance comes into play.
A relatively new yet crucial field, technovigilance is all about keeping a close watch on medical devices after they hit the market, making sure they are safe, effective, and reliable for all users. In this blog post, we will explore the importance of technovigilance, its key components, the challenges it faces, and best practices for manufacturers and healthcare providers to ensure the highest standards of safety and efficacy.
What is Technovigilance?
Technovigilance is a comprehensive set of standards, mechanisms, processes, and resources dedicated to the identification, evaluation, and management of adverse events and technical complaints associated with medical devices and health-related products. These products range from medical equipment and hospital supplies to implants and in-vitro diagnostic tools.
Unlike pre-market assessments, which focus on evaluating devices before they are introduced to the public, technovigilance emphasizes the post-marketing phase, where real-world data and user experiences are critical for ongoing safety assessment.
A key component of technovigilance involves complying with established regulations, such as the COUNCIL DIRECTIVE 93/42/EEC of 14 June 1993, which sets out the legal obligations for manufacturers regarding the monitoring and reporting of adverse effects related to their health products.
This directive mandates not only the detection and documentation of any undesirable effects but also their prompt reporting to competent authorities. This rigorous approach ensures that issues are addressed swiftly, minimizing potential harm to patients and users while maintaining public trust in medical devices.
The Growing Need for Technovigilance
The scope of technovigilance is vast and ever-growing. According to the 'Global Atlas of Medical Devices' published by the World Health Organization (WHO) in 2017, there were an estimated 2 million different types of medical devices available on the global market. These are categorized into various device groups, each with unique properties, potential benefits, and risks.
With the rapid technological advancements expected in the coming years, this number is only set to increase, adding layers of complexity to the already challenging task of health product surveillance.
The sheer diversity and rapid innovation in medical devices make technovigilance an exceptionally specialized area. It requires not just a superficial understanding but in-depth knowledge across multiple domains—scientific, technical, legal, and clinical. As such, a multidisciplinary approach is critical.
Teams comprising scientists, engineers, healthcare professionals, regulatory experts, and legal advisors must collaborate closely to ensure a robust surveillance system that can keep pace with the dynamic landscape of medical technology.
Why is Technovigilance So Crucial Today?
In an era where healthcare technology is becoming increasingly sophisticated, the margin for error must be minimized. Technovigilance serves as the frontline defense in ensuring that the advanced medical devices meant to improve and save lives do not inadvertently cause harm.
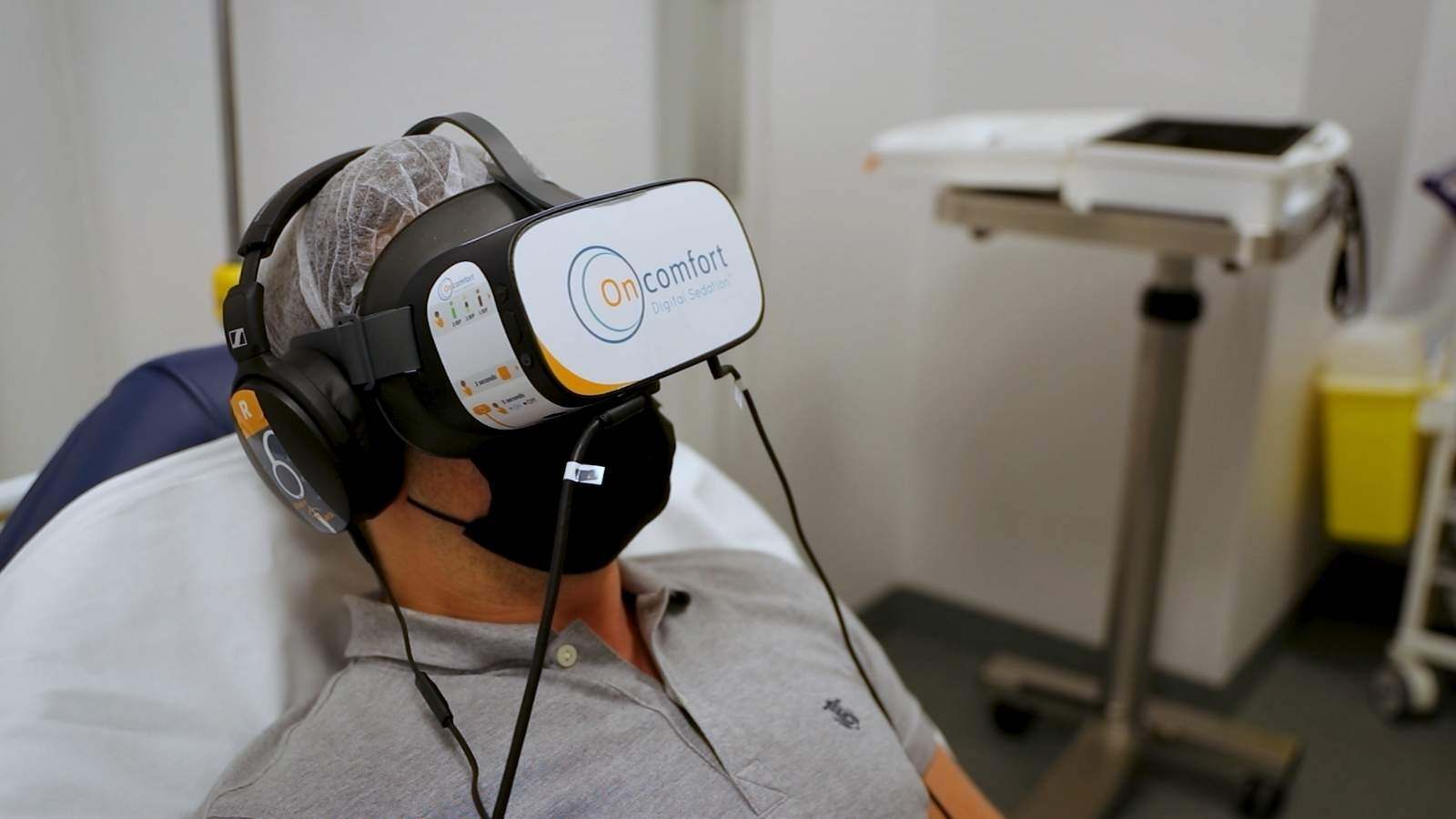
With technologies like AI-driven diagnostic tools, wearable health monitors, and smart implants entering the market, the potential for both positive impact and unforeseen risks has never been higher. This dual potential reinforces the need for rigorous technovigilance practices.
The importance of technovigilance cannot be understated—it’s not just about addressing problems after they arise but also about anticipating and preventing them. This proactive stance helps build trust with consumers and stakeholders, ensuring that innovations in medical technology translate into genuine health benefits rather than new categories of risk.
Key Challenges in Technovigilance
While technovigilance is crucial, it also comes with its set of challenges. Below are some of the most pressing challenges faced by the industry:
Data Privacy and Security Concerns
One significant challenge is data privacy and security. As technovigilance relies heavily on collecting and analyzing data from various sources—ranging from healthcare providers to real-time data from IoT-enabled medical devices—ensuring the confidentiality and security of this data is paramount. Breaches or mishandling of sensitive patient information can lead to legal consequences and erode public trust.
Under-Reporting of Adverse Events
Another challenge is the under-reporting of adverse events. Many healthcare providers may not report minor issues, or there could be delays in reporting due to bureaucratic hurdles or lack of awareness. This under-reporting can skew data, making it harder to identify potential risks early on.
Diverse Global Regulations
The global diversity in regulations poses a significant hurdle. Different countries have different standards, reporting requirements, and monitoring systems, making it challenging for manufacturers operating in multiple markets to maintain compliance across all jurisdictions. The lack of a globally harmonized regulatory framework can lead to discrepancies and gaps in surveillance.
Best Practices for Manufacturers and Healthcare Providers
To overcome these challenges, it’s essential for manufacturers and healthcare providers to adopt best practices in technovigilance:
1. Establish a Robust Reporting System
Develop a streamlined system that encourages the timely reporting of adverse events and technical complaints. Training staff on the importance of reporting and how to do it efficiently can significantly reduce under-reporting.
2. Leverage Technology for Data Analysis
Utilize advanced data analytics and machine learning tools to analyze data from various sources, identify patterns, and predict potential risks before they escalate. Investing in these technologies can provide a proactive approach to risk management.
3. Ensure Compliance Across Markets
For global manufacturers, understanding and complying with different regional regulations is crucial. This may require dedicated teams or consultants who specialize in regulatory affairs for each region.
4. Focus on Data Privacy and Security
Implement strong data protection measures to ensure that patient data and sensitive information are safeguarded. This includes regular audits, encryption, and ensuring compliance with data privacy laws like GDPR.
5. Foster a Multidisciplinary Approach
A successful technovigilance program requires collaboration among various experts, including regulatory professionals, scientists, engineers, and legal advisors. Establishing a multidisciplinary team ensures a comprehensive approach to managing potential risks.
Partnering for Excellence in Technovigilance
The complex landscape of technovigilance demands a strategic approach and expert guidance. This is where partnering with specialists can make a significant difference.
By collaborating with experienced professionals, manufacturers and healthcare providers can more effectively address these challenges, ensuring that their surveillance systems are both robust and compliant across diverse markets.
At QbD Group, we specialize in comprehensive technovigilance solutions tailored to meet the unique needs of our clients.
Our experts are well-versed in the nuances of regulatory requirements, risk management, and technological surveillance, ensuring that you are always a step ahead in maintaining compliance and protecting consumer well-being.
Whether you have questions about specific technovigilance processes or need end-to-end support to navigate this complex field, we’re here to help.







.png?width=109&height=108&name=Pharma%20(2).png)
.png?width=111&height=108&name=Medical%20Devices%20(2).png)
.png?width=84&height=107&name=IVD%20(2).png)




















%20Checklist.jpg)










.jpg)




.jpg)

















.jpg)

.jpg)


.png)

.jpg)
.jpg)


.jpg)
.jpg)

.jpg)
.png)