Sterilization validation is a vital process in the healthcare and pharmaceutical industries. It ensures that sterilization methods are not just effective but consistently reliable, making sure products are free from harmful microorganisms.
In this blog post, we’ll break down why sterilization validation is essential, the steps involved, and how to navigate common challenges.
Sterilization validation is a documented process that confirms that a sterilization process consistently produces products that meet pre-determined Sterility Assurance Levels (SAL). It involves rigorous testing and documentation to ensure that the sterilization method is effective and reliable.
Sterilization validation plays a vital role in several areas. Here’s why it is crucial:
- Patient Safety: Ensuring that medical devices, pharmaceuticals, and other healthcare products are sterile is crucial for patient safety. Contaminated products can lead to infections and other serious health issues.
- Regulatory Compliance: Regulatory bodies such as the FDA and EMA require stringent validation of sterilization processes to ensure product safety and efficacy.
- Quality Assurance: Validation helps maintain high standards of quality, ensuring that products are consistently safe for use.
5 Key Steps in Sterilization Validation
Sterilization validation consists of several key steps to ensure that the sterilization process is both effective and reliable. The main steps include:
1. Selection of Sterilization Method
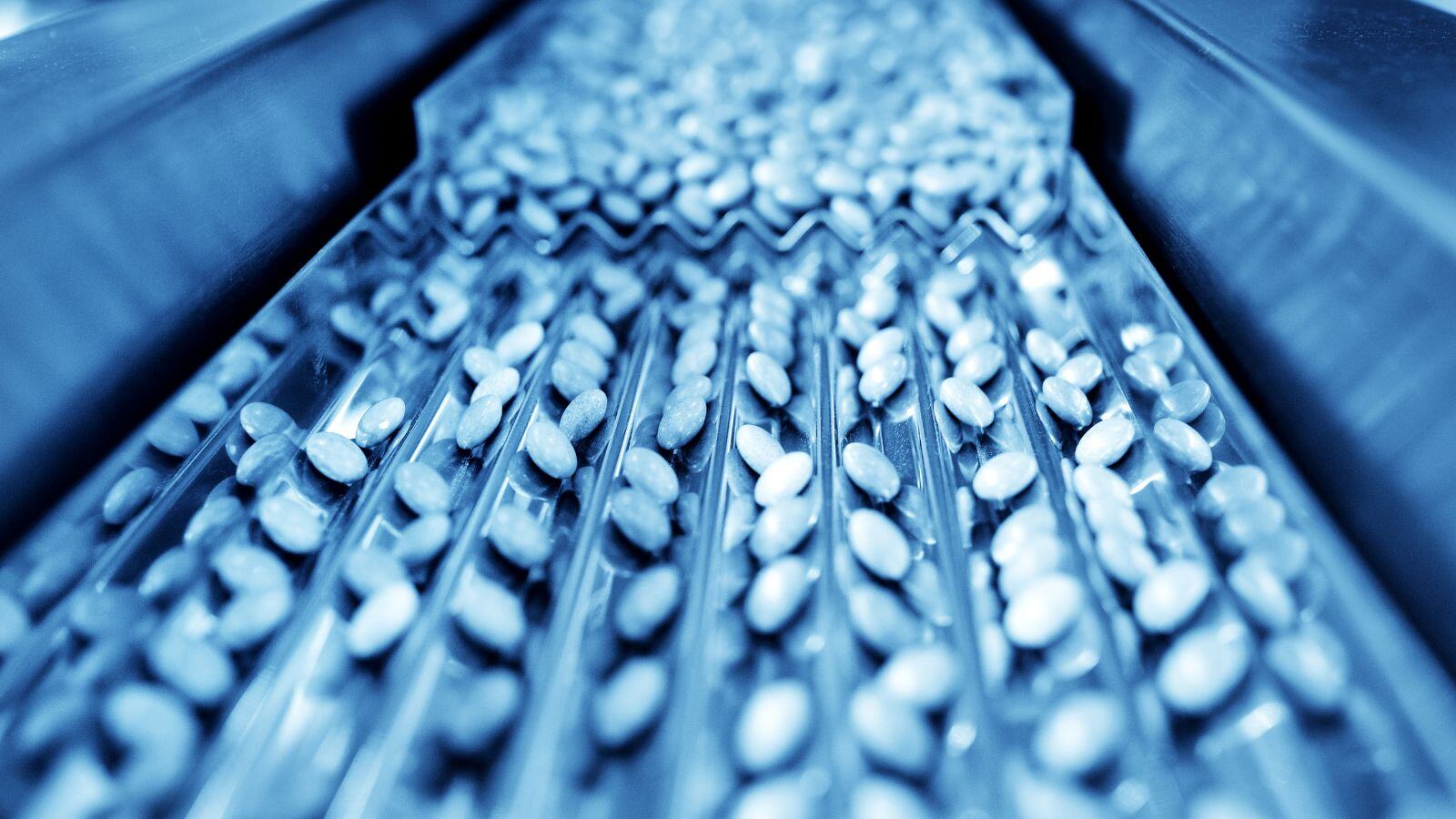
Choose an appropriate sterilization method based on the nature of the product. Common methods include steam sterilization, ethylene oxide (EtO) sterilization, and radiation sterilization.
|
Type of Sterilization
|
When to Use
|
|---|---|
|
Steam
|
In Place (SIP) for production equipment without prior disassembly. Out of Place (autoclave) for small, heat-resistant materials (e.g., glassware, surgical instruments), culture media, packaging materials, and end sterilization of heat-stable pharmaceutical products.
|
|
Ethylene Oxide (EtO)
|
For heat- and moisture-sensitive products (e.g., medical devices, electronics).
|
|
Radiation
|
For large-scale sterilization (e.g., single-use medical devices, packaging materials).
|
|
Dry Heat
|
For materials that can withstand high temperatures but are sensitive to moisture (e.g., powders, oil).
|
|
Filtration
|
For heat-sensitive liquids and gases (e.g., injectable drugs, solutions).
|
|
Vaporized Hydrogen Peroxide (VHP)
|
For sterilizing medical devices, equipment, and surfaces in healthcare settings.
|
Table 1: Overview of the most common sterilization methods.
The FDA and EMA prefer terminal sterilization methods (e.g., steam, radiation) whenever possible due to their reliability and effectiveness. Aseptic processing is used when terminal sterilization is not feasible.
2. Installation Qualification (IQ)
Verify that the sterilization equipment is installed correctly and operates according to the manufacturer’s specifications. This ensures that all utilities (e.g., steam, water, electricity) are properly connected and meet the required specifications.
Instruments and sensors (e.g., temperature, pressure gauges) must also be calibrated and functional. Safety tests are also performed to ensure operational readiness.
3. Operational Qualification (OQ)
Test the equipment under normal operating conditions to ensure it performs as expected. Key tests include empty chamber temperature mapping (for steam and dry heat sterilization), alarm conditioning tests, and cycling verification.
4. Performance Qualification (PQ)
This phase involves testing to confirm that the sterilization process consistently produces sterile products. Key activities include simulated load temperature mapping (for steam and dry heat sterilization), the use of biological or chemical indicators (depending on the sterilization method), as well as penetration testing, sterilant residue testing, and endotoxin testing.
Biological and chemical indicators play a crucial role in challenging the sterilization process. Biological indicators, in particular, contain highly resistant microorganisms to verify that the sterilization process is truly effective.
5. Documentation and Reporting
Maintain thorough documentation of all validation activities, including test results, protocols, and any deviations. This documentation is essential for regulatory compliance and quality assurance.
Challenges in Sterilization Validation
Despite its importance, sterilization validation poses several challenges. Here’s an overview of some common challenges:
Complex Product Designs
Medical devices with intricate designs or materials that are sensitive to heat or chemicals can be difficult to sterilize effectively. Ensuring that the sterilization process reaches all parts of the device without damaging it is a significant challenge.
Consistency and Reproducibility
Achieving consistent and reproducible results across different batches and production runs is critical. Variability in the sterilization process can result in non-sterile products, putting patient safety at risk. Possible root causes include improper loading, equipment malfunction, environmental factors (e.g., humidity, airflow, temperature), or human error.
Validation of New Sterilization Methods
As new sterilization technologies and methods are developed (e.g., gas plasma technology for medical devices, ozone sterilization), the validation of these new processes to meet regulatory standards can be complex and resource-intensive. This includes demonstrating that new methods are as effective as traditional ones.
Biological Indicator Performance
Using biological indicators to challenge the sterilization process can be difficult, especially when dealing with highly resistant microorganisms. Ensuring that these indicators accurately reflect the effectiveness of the sterilization process is critical.
Regulatory Compliance
Keeping up with evolving regulatory requirements can be demanding, requiring constant updates to validation protocols. For instance, the 2023 EPA proposal requiring commercial sterilization facilities to comply within 18 months with stricter emission and control standards for ethylene oxide (EtO) has had a serious impact on the validation process.
Resource Constraints
The sterilization validation process can be time-consuming and resource-intensive, requiring specialized equipment and expertise. Smaller companies, in particular, may struggle with the financial and logistical demands of thorough validation.
Sterilization validation is a crucial part of ensuring the safety and efficacy of healthcare products. By following rigorous validation protocols, manufacturers can ensure their products meet the highest standards of sterility, protecting patient health and maintaining regulatory compliance.
As new technologies and stricter regulations continue to evolve, keeping your validation processes up to date is more important than ever.
Do you need expert help with designing or validating your sterilization process?
Our team of experts is ready to support you, whether you need help addressing sterilization issues or ensuring regulatory compliance.








.jpg)